IOL calculation before / after DMEK surgery
Descemet membrane endothelial keratoplasty (DMEK) was introduced in 2006 by Melles et al (1). This procedure revolutionized the management of endothelial pathologies by allowing a near perfect anatomical replacement of the diseased endothelium.
In most of the cases, the diseased (pre-DMEK) posterior corneal surface is (fortunately !) not taken into account in IOL formula calculations. As this posterior surface is restored back to its physiological shape by DMEK surgery, precise IOL calculation in triple procedure (i.e. prediction of the adequate IOL power for a post-DMEK eye using measurements made on a pre-DMEK eye) should be possible without any surprise.
However, a so-called "hyperopic shift" is observed both in standalone DMEK and in DMEK triple procedure. Why ? What is the difference between those phenomena ?
Hyperopic shift in DMEK standalone procedure
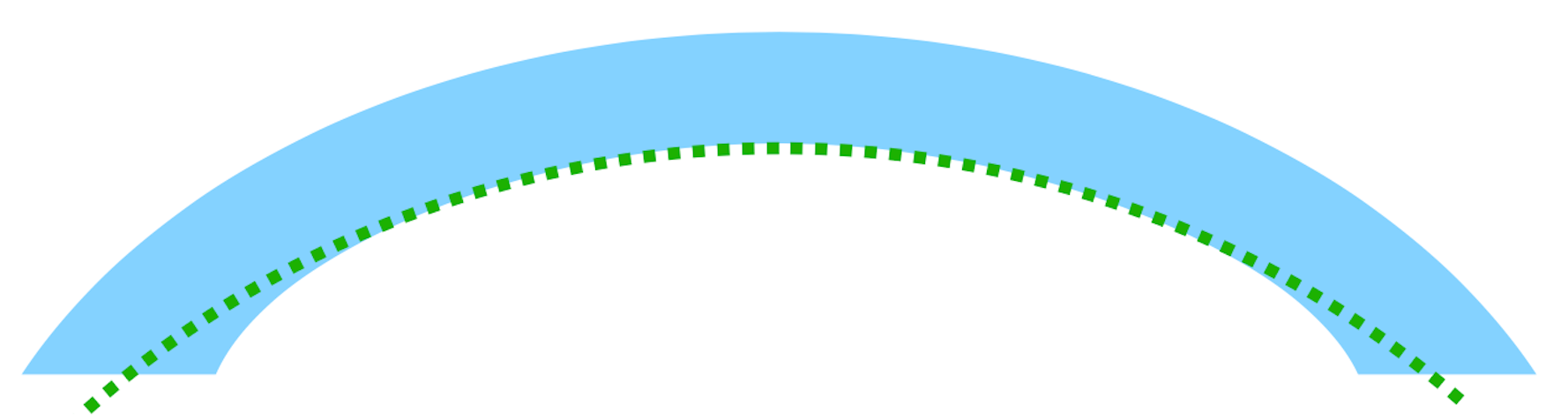
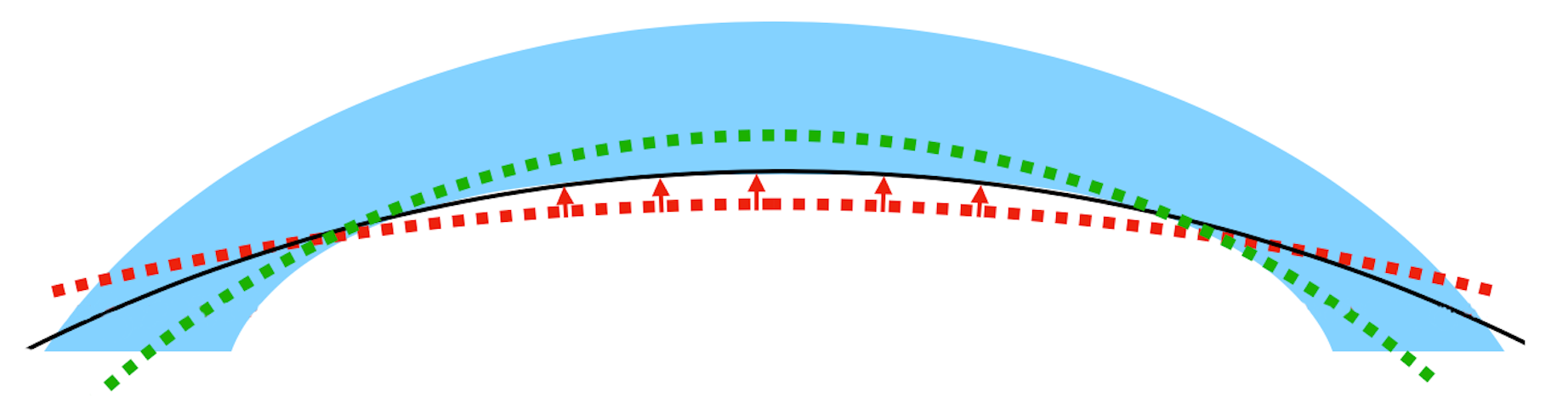
The refractive shift observed in DMEK single procedure is logical and easy to understand. The pathological, flattened posterior corneal surface is restored to its physiological value by the surgery. The posterior corneal radius decreases, thus decreasing the corneal power*. The eye is more hyperopic after the surgery (2-4).
*An increase in anterior corneal radius decreases the corneal power ; an increase in posterior corneal radius increases the corneal power.
Does this phenomenon have an impact in IOL calculation? Theoretically, no : let's see why.
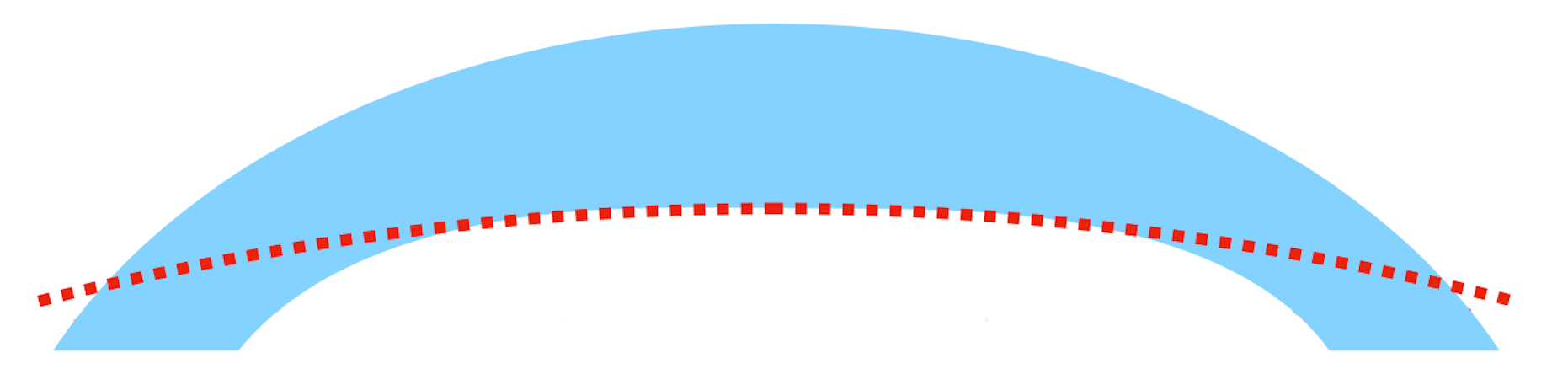
Restoring the posterior corneal surface to its physiological value does not impact IOL calculation
As explained in 2011 by Ham et al. (5), biometric measurements do not usually take into account the posterior corneal radius. The corneal power is extrapolated from the anterior corneal radius, and (it was initially thought that) no modification of the anterior corneal radius happens after DMEK surgery. If the anterior radius is not modified and the posterior radius goes back to its physiological value, a refractive shift (in a single procedure) should be observed, but no IOL calculation error (in DMEK triple procedure) should occur.
Note : Of course this is not true for ray-tracing methods or total corneal power calculations using a measured posterior corneal radius, available in the most recent biometers. Those methods should by avoided at all costs in DMEK-triple procedure, because the posterior corneal radius will change after DMEK surgery.
Since 2011, various authors have in fact described a modification of the anterior corneal radius, and steeper-than-normal posterior corneal radii (6-11); IOL calculation error in triple-DMEK has also been well described by different teams (12-15). If the anterior radius is indeed different at the time of the biometry and after DMEK, it is logical to observe an error. Similarly, if the posterior corneal radius is steeper-than-normal after DMEK, the usual relationship between the anterior radius and the posterior radius is no longer valid and standard keratometric indices will be flawed. Both phenomena can explain an IOL calculation error.
As explained in a recent paper by our team, it is then necessary to distinguish two different phenomena (17) :
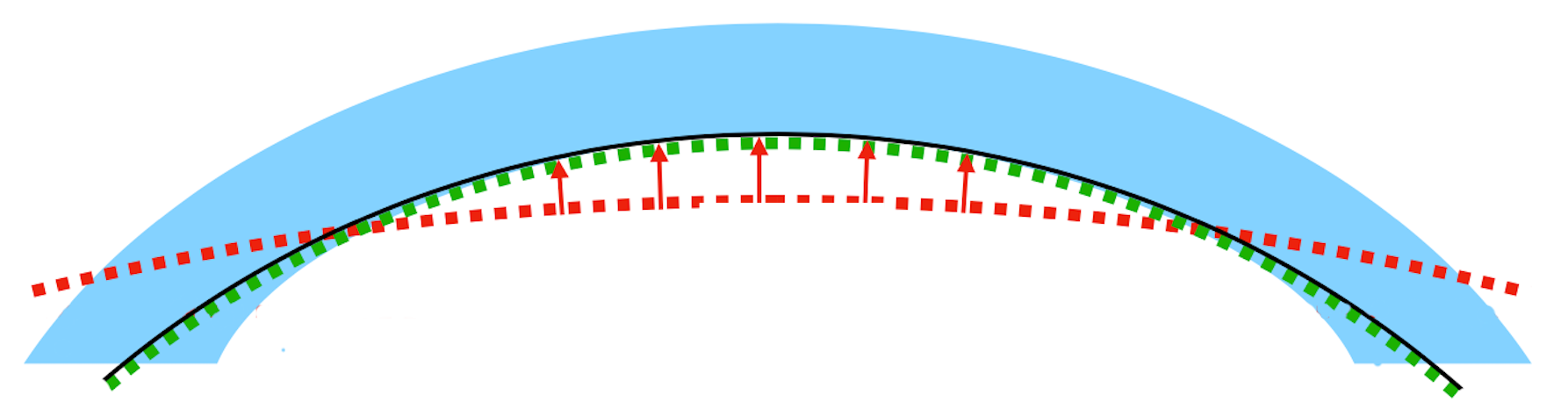
- DMEK-induced refractive shift (DIRS) : the (usually hyperopic) refractive shift observed in standalone procedure, which is explained by the difference between the pre-DMEK corneal power and the post-DMEK corneal power. It is a pure modification of corneal power.
- DMEK-induced IOL calculation error (DICE) : the IOL calculation error happening because of anterior corneal radius modifications before and after DMEK, and non-physiological post-DMEK posterior radii. It is the difference between the corneal power estimated by IOL formulas using pre-DMEK measurements and the real post-DMEK corneal power. IOL formulas are flawed because the anterior radius changes (or is incorrectly measured pre-DMEK), or because the anterior/posterior relationship is broken, or both.
Surprisingly, both phenomena are usually referred to as "hyperopic shift" in the literature. They should be differentiated !
NB : it could also be hypothesized that the refractive index of the cornea is also non-physiological after DMEK. This phenomenon is very difficult to isolate in clinical practice, but could also partly explain both DIRS and DICE.
Relative impact of anterior and posterior corneal radii variations on corneal power
Anterior and posterior corneal radii variations both influence the corneal power. But what is the relative importance of both phenomena ?
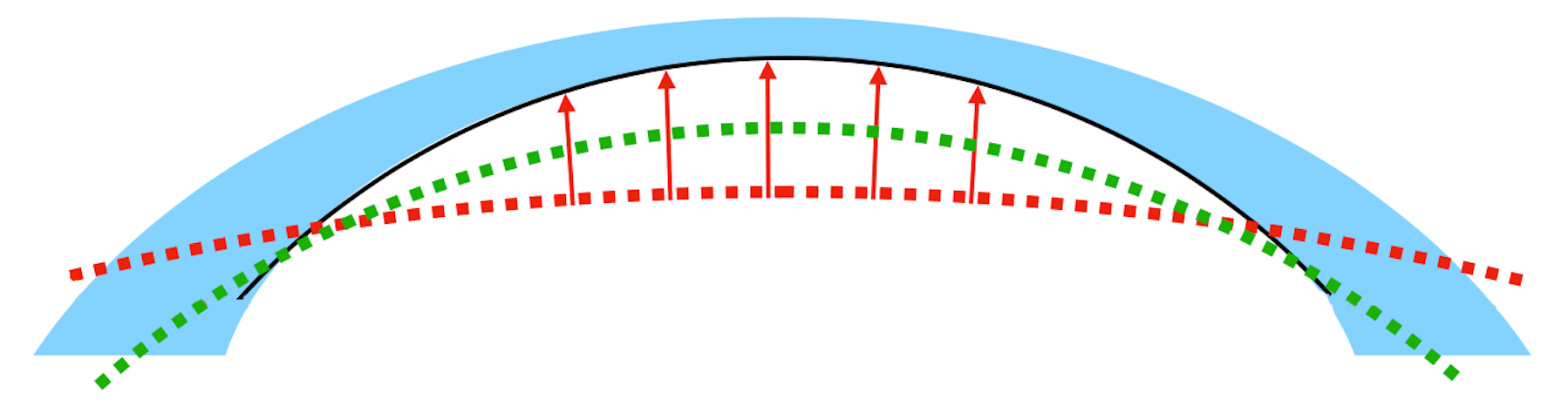
It should be remembered that the difference between the refractive index of the air (n_air = 1) and of the cornea (n_cor = 1.376) is much greater than the difference between the refractive index of the cornea and of the aqueous (n_aq = 1.336) : 0.376 and 0.04, respectively.
For a theoretical cornea (ARC = 7.5mm, PRC = 6.5mm, CCT = 0.520mm), a variation of 0.1mm in ARC leads to a difference in corneal power of 0.68D, while a the same variation of PRC modifies it by 0.1D. This is almost a sevenfold difference!

Is it possible to predict the variation in anterior corneal radius and/or the post-DMEK anterior/posterior ratio ?
DIRS can't be prevented : the corneal power will always be modified by DMEK surgery. By contrast, DICE could theoretically be avoided (by correcting the IOL calculation) if its underlying mechanisms were clearly understood.
Flatter and more oblate posterior corneal surfaces, as well as a higher posterior to anterior corneal curvature radii ratio have been cited as DIRS or DICE risk factors (8,15,16).
In a recent study (17), we did not find any strong predictor for DIRS or DICE. However, we found, like Schoenberg et al. (14), a lower variation of the ARC measured before and after DMEK when using a Scheimpflug camera, compared to the measurement obtained with the IOLMaster. Could the "variation" in ARC be partly explained by an ARC measurement error made by our biometers, which could be lowered by using the ARC measured by Scheimpflug camera in our IOL formulas ?
Conclusion
- DIRS is the DMEK-induced variation in corneal power, observed in DMEK single procedure, which can't be avoided. Any anterior or posterior corneal radius modification induces a DIRS. It is not preventable.
- DICE is the IOL calculation error induced by modifications/measurement errors of the ARC, and/or non-physiological post-DMEK posterior corneal radii. Any anterior corneal radius modification induces a DICE, but, unlike DIRS, posterior corneal radius modifications are involved in DIRS only when this radius is non-physiological after DMEK. It is theoretically preventable.
- It could be wise to aim for a more myopic target when the posterior corneal surface is very flat and oblate. The ARC value measured using the Pentacam device should be preferred to the ARC value obtained using a biometer. However, no strong DICE predictor has been found to date.
References :
- Melles GR. Posterior lamellar keratoplasty: DLEK to DSEK to DMEK. Cornea. 2006 Sep;25(8):879-81.
- Dunker SL, Veldman MHJ, Winkens B, van den Biggelaar FJHM, Nuijts RMMA, Kruit PJ, Dickman MM; Dutch Cornea Consortium. Real-World Outcomes of DMEK: A Prospective Dutch registry study. Am J Ophthalmol. 2021 Feb;222:218-225.
- Price MO, Giebel AW, Fairchild KM, Price FW Jr. Descemet's membrane endothelial keratoplasty: prospective multicenter study of visual and refractive outcomes and endothelial survival. Ophthalmology. 2009
- Agha B, Ahmad N, Dawson DG, Kohnen T, Schmack I. Refractive outcome and tomographic changes after Descemet membrane endothelial keratoplasty in pseudophakic eyes with Fuchs' endothelial dystrophy. Int Ophthalmol. 2021 Aug;41(8):2897-2904.
- Ham L, Dapena I, Moutsouris K, Balachandran C, Frank LE, van Dijk K, Melles GR. Refractive change and stability after Descemet membrane endothelial keratoplasty. Effect of corneal dehydration-induced hyperopic shift on intraocular lens power calculation. J Cataract Refract Surg. 2011 Aug;37(8):1455-64.
- Alnawaiseh M, Rosentreter A, Eter N, Zumhagen L. Changes in Corneal Refractive Power for Patients With Fuchs Endothelial Dystrophy After DMEK. Cornea. 2016 Aug;35(8):1073-7.
- Arnalich-Montiel F, Mingo-Botín D, Diaz-Montealegre A. Keratometric, Pachymetric, and Surface Elevation Characterization of Corneas With Fuchs Endothelial Corneal Dystrophy Treated With DMEK. Cornea. 2019;38:535-541.
- Cheung AY, Chachare DY, Eslani M, et al. Tomographic changes in eyes with hyperopic shift after triple Descemet membrane endothelial keratoplasty. J Cataract Refract Surg. 2018;44:738-744.
- Parker J, Dirisamer M, Naveiras M, et al. Outcomes of Descemet membrane endothelial keratoplasty in phakic eyes. J Cataract Refract Surg. 2012;38:871-877.
- van Dijk K, Ham L, Tse WHW, et al. Near complete visual recovery and refractive stability in modern corneal transplantation: Descemet membrane endothelial keratoplasty (DMEK). Cont Lens Anterior Eye. 2013;36:13-21.
- van Dijk K, Rodriguez-Calvo-de-Mora M, van Esch H, et al. Two-Year Refractive Outcomes After Descemet Membrane Endothelial Keratoplasty. Cornea. 2016;35:1548-1555.
- Augustin VA, Weller JM, Kruse FE, Tourtas T. Refractive Outcomes After Descemet Membrane Endothelial Keratoplasty + Cataract/Intraocular Lens Triple Procedure: A Fellow Eye Comparison. Cornea. 2021 Jul 1;40(7):883-887
- Bae SS, Ching G, Holland S, McCarthy M, Ritenour R, Iovieno A, Yeung SN. Refractive Outcomes of Descemet Membrane Endothelial Keratoplasty Combined With Cataract Surgery in Fuchs Endothelial Dystrophy. J Refract Surg. 2020 Oct 1;36(10):661-666.
- Schoenberg ED, Price FW Jr, Miller J, et al. Refractive outcomes of Descemet membrane endothelial keratoplasty triple procedures (combined with cataract surgery). J Cataract Refract Surg. 2015;41:1182-1189.
- Fritz M, Grewing V, Böhringer D, et al. Avoiding Hyperopic Surprises After Descemet Membrane Endothelial Keratoplasty in Fuchs Dystrophy Eyes by Assessing Corneal Shape. Am J Ophthalmol. 2019;197:1-6.
- Diener R, Eter N, Alnawaiseh M. Using the posterior to anterior corneal curvature radii ratio to minimize the risk of a postoperative hyperopic shift after Descemet membrane endothelial keratoplasty. Graefes Arch Clin Exp Ophthalmol. January 2020.
- Debellemanière G, Ghazal W, Dubois M, et al. Descemet Membrane Endothelial Keratoplasty–Induced Refractive Shift and Descemet Membrane Endothelial Keratoplasty–Induced Intraocular Lens Calculation Error. Cornea 2022.